The lower eyelid is among the most unforgiving areas in aesthetic surgery. Even small miscalculations in flap design, dissection, or resection can result in complications such as ectropion, scleral show, hollowing, or a fatigued appearance.
For this reason, a detailed understanding of eyelid anatomy — coupled with precise operative planning — is essential before choosing between a skin–muscle flap or a skin-only flap blepharoplasty.
Anatomical Review
The lower eyelid is composed of multiple layers, each with critical surgical implications:
Skin: the thinnest in the body, with minimal subcutaneous tissue, making it vulnerable to scarring and retraction.
Orbicularis oculi muscle: divided into preseptal and orbital portions. It provides dynamic support to the lid and contributes to tone. Weakness or laxity here predisposes to malposition after surgery.
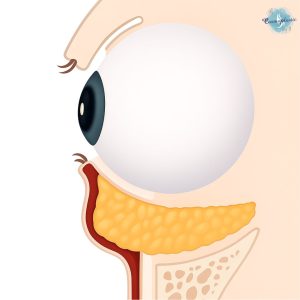
Orbital septum: a fibrous layer attaching to the arcus marginalis, separating the orbicularis from the fat pads. Age-related attenuation allows orbital fat herniation, forming the classic “bags.”
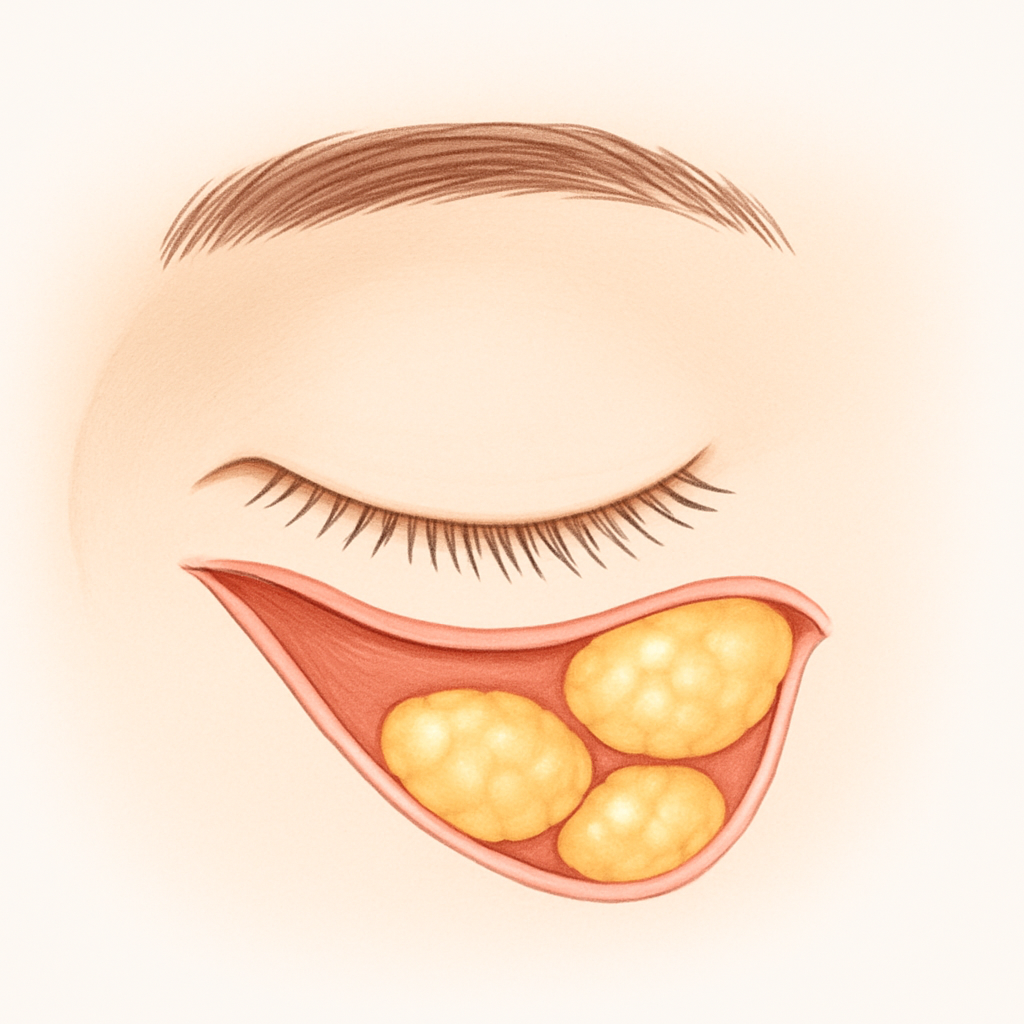
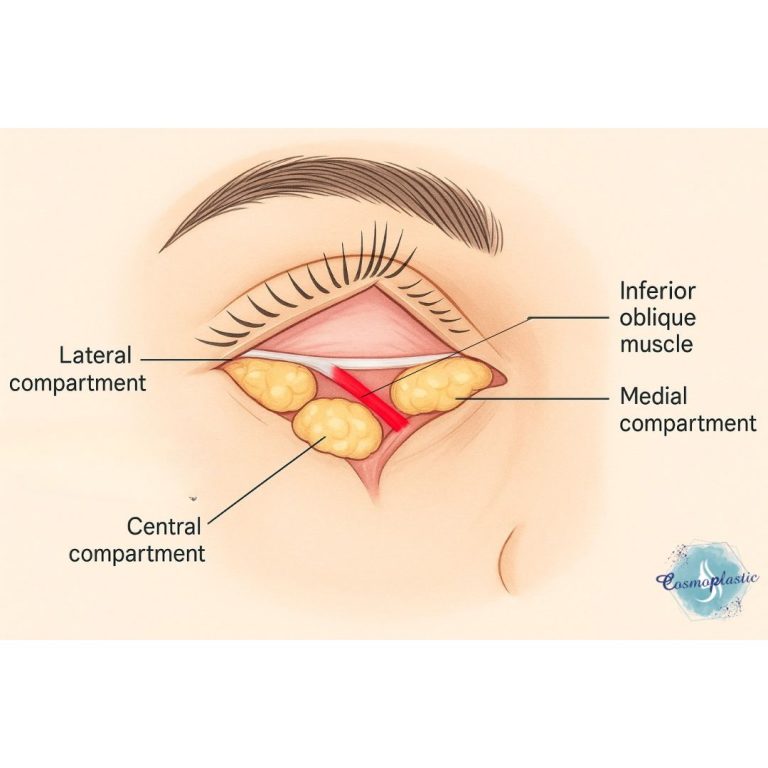
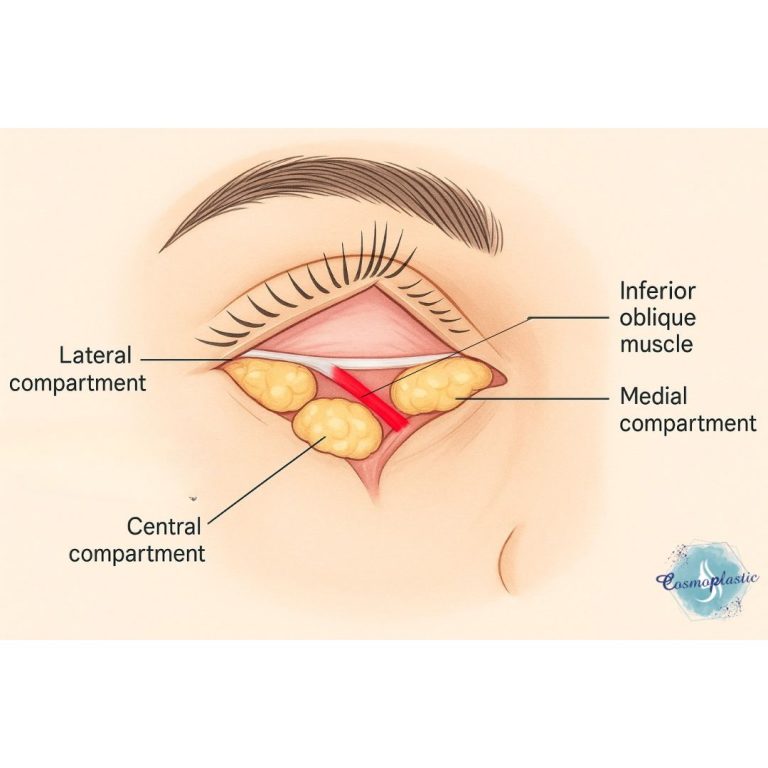
Fat pads: three discrete compartments (medial, central, lateral). Understanding their topography is essential for selective removal or repositioning.
Tarsal plate and canthal tendons: structural pillars of eyelid stability. Injury or over-dissection near these landmarks risks long-term functional compromise.
Retaining ligaments: particularly the orbicularis retaining ligament and the tear trough ligament, which anchor the orbicularis and define the lid–cheek junction. Their prominence contributes to the hollow transition that often drives patient concerns.
This layered anatomy explains why lower blepharoplasty cannot be approached with a “one size fits all” mindset.
Skin–Muscle Flap Approach
The skin–muscle flap involves elevating the skin and orbicularis together in a composite flap, typically via a subciliary incision.
Operative principles:
The dissection begins just below the lash line, with careful elevation of skin and orbicularis as a single unit in the sub–orbicularis plane.
Fat pads are then exposed by incising the septum, allowing selective excision or transposition.
The orbicularis is often resuspended laterally to the lateral canthal tendon, reinforcing tone and reducing postoperative descent.
Skin is conservatively trimmed, with care to avoid over-resection.
Advantages:
Allows direct access to orbicularis laxity and festoons.
Facilitates blending of the lid–cheek junction by releasing retaining ligaments and repositioning fat.
Provides more powerful redraping in cases with muscle redundancy.
Limitations and risks:
Greater tissue trauma with more swelling and longer recovery.
Higher risk of postoperative lid malposition (ectropion, retraction) if flap tension is excessive or orbicularis support is not restored.
Technically more demanding, requiring meticulous haemostasis and layered closure.
This approach is best reserved for patients with orbicularis laxity, festoons, or significant tear trough deformity, where deeper support must be addressed.
Skin-Only Flap Approach
The skin-only technique involves raising skin separately, leaving orbicularis undisturbed.
Operative principles:
A subciliary incision is made just below the lash line.
Dissection proceeds immediately beneath the skin, sparing the orbicularis.
Redundant skin is excised conservatively.
If fat herniation is present, it may be addressed through a transconjunctival approach in combination.
Advantages:
Minimal disruption of orbicularis, preserving tone and function.
Reduced swelling and faster recovery.
Lower risk of postoperative lid malposition compared to the skin–muscle flap.
Limitations:
Limited ability to address orbicularis laxity or festoons.
Less effective in correcting lid–cheek transition irregularities.
Reliant on preoperative orbicularis tone — unsuitable for patients with weakness or significant muscle redundancy.
The skin-only flap is best suited for patients with strong orbicularis support and isolated skin redundancy.
Surgical Judgment: Choosing the Right Approach
The decision between these techniques is rarely straightforward. Key considerations include:
Orbicularis tone: strong tone favors skin-only, while laxity necessitates a skin–muscle flap.
Patient age and anatomy: younger patients often benefit from the conservative skin-only approach, while older patients with festoons or muscle laxity may require skin–muscle work.
Fat management: skin-only is limited in addressing fat; skin–muscle allows direct access and repositioning.
Risk tolerance: surgeons must weigh the potential for more dramatic rejuvenation against the higher risk of malposition.
Operative Pearls
✔️ Always perform a preoperative pinch test to guide safe skin excision.
✔️ In skin–muscle flaps, lateral canthal support (e.g., orbicularis suspension, canthopexy) is critical to prevent descent.
✔️ Avoid over-resection of skin — the most common error leading to retraction and ectropion.
✔️ Consider combining transconjunctival fat management with skin-only excision for a balanced approach in selected patients.
Read Next